Hepatitis C During Pregnancy: Risks And Treatment – You Are Parents
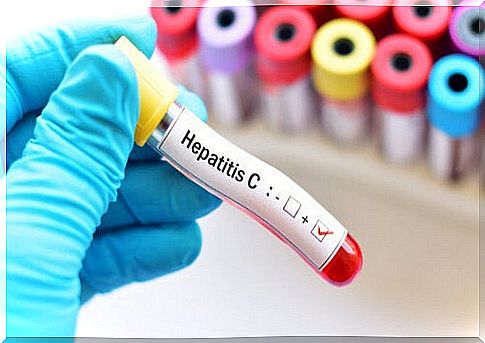
Hepatitis C in pregnancy is a public health problem, although complications occur in a small proportion of patients. It is a viral infection that is widespread in the world and is transmitted through the blood, in particular through the injection of illicit drugs.
While there is no increased risk of complications during pregnancy, some pregnant women and babies may experience additional difficulties due to chronic infection. If you would like to know a little more about the subject, we invite you to read on.
What is hepatitis C?
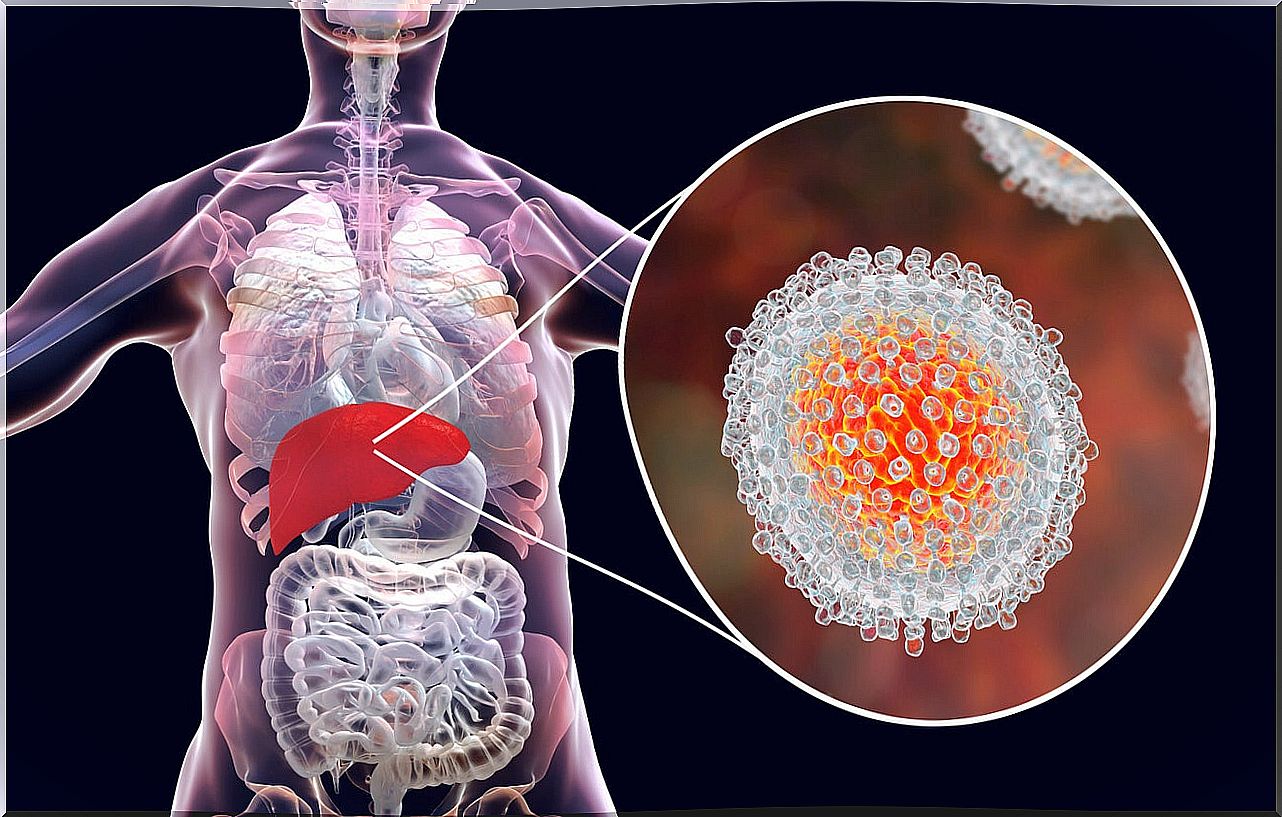
As the name suggests, hepatitis C is a disease characterized by inflammation of the liver tissue. Which, in turn, is caused by the hepatitis C virus. According to a publication from the World Health Organization (WHO), the virus can cause chronic infection. Although, in most cases, those affected are asymptomatic.
This last point does not imply that the disease is mild every time. This is because it is a major cause of liver cancer in people living with a chronic infection. An estimated population of 71 million people, according to the WHO.
Although the distribution of the virus and disease is global, it is more common in parts of Europe and the eastern Mediterranean. Particularly among at-risk groups who tend to use illicit injection drugs.
How is it transmitted?
Blood is the fluid through which disease is transmitted. According to a scientific journal article published in the journal Offarm: Pharmacy and Society , the most frequent routes are as follows:
- Transfusions.
- Hemodialysis.
- Parenteral drug addiction.
- Organ transplantation.
- Work accidents among health personnel.
- Tattoos, acupuncture and piercing .
Another important transmission route is the vertical route. That is, the one that occurs from mother to child during pregnancy.
According to a publication by the Argentine Federation of Obstetrics and Gynecological Societies, in the United States between 1 and 2.5% of pregnant women are infected. This greatly increases the risk of vertical transmission.
How do I know if I have hepatitis C?
From a clinical point of view, most patients are asymptomatic, especially in acute infections. When symptoms do appear, it is always after the incubation period of the virus, which can range from 2 weeks to 6 months. The most common are the following:
- Yellowing of the skin (jaundice).
- Loss of appetite.
- Nausea and vomiting.
- Abdominal pain, especially in the upper and right part (upper right quadrant).
- Fever.
- Dark urine.
- Pale or clear stools.
If the presentation of one of these symptoms, it is important to go as soon as possible to the doctor to make the diagnosis of hepatitis C. In any case, in some countries it is advisable to perform periodic tests, especially during antenatal visits.
These diagnostic studies include blood tests, which are serological tests that determine the amount of antibodies to the virus in the blood. If these are high, there is a confirmatory test that determines the presence of the virus’s genetic material in the blood.
If the latter test is positive and doctors need to assess the severity of the liver damage, they may order a liver elastogram, MRI, transient elastography, or liver biopsy. This is how the experts at the Mayo Clinic describe it in a publication.
Treatment of hepatitis C during pregnancy
Treatment during pregnancy varies depending on the symptoms and the degree of liver failure. According to a publication in the Journal of Gastroenterology of Peru , therapy in these cases serves several purposes:
For this reason, simply avoiding any hepatotoxic medication can be used to prevent complications from the infection. Women with cirrhosis of the liver (a consequence of chronic hepatitis) can experience many difficulties that require emergency treatment.
This includes drugs to prevent clotting as well as endoscopic or surgical procedures to treat varicose veins that can cause internal bleeding.
Hepatitis C and pregnancy: how does it affect you and your baby?
Many women can go through a pregnancy without knowing they have hepatitis C. The risk of developing complications is low. However, in some predisposing people, chronic infection can progress to cirrhosis of the liver and cancer.

Although vertical transmission of the virus is a possibility, there is so far no evidence to suggest that elective cesarean sections or interruption of breastfeeding decrease the risk of infection of the baby.
A study entitled Transmission of the hepatitis C virus to the newborn describes that the risks of infection are highest during childbirth, with no significant difference between cesarean section and the natural route. In addition, co-infection with HIV appears to increase the risk of transmission.
Chronic hepatitis C virus infection does not pose additional risks during pregnancy, according to a book published in Gastroenterology and Hepatology . If the mother is in clinically stable condition, the biggest problem that can arise is infection of the baby through the aforementioned routes.
In this case, although acute infection can generate alarming symptoms, it is the low possibility of chronic infection that can have the greatest impact on children’s health. For this, regular medical examinations are essential.
Medical follow-up is essential
Although in the vast majority of cases, hepatitis C does not cause significant health problems, it should be taken into account that it is a disease that can develop complications.
For this reason, it is important to access screening tests or see a doctor if any of the symptoms present for early diagnosis and prompt treatment.